Glial cell transplantation is emerging as a promising therapeutic strategy for neurodegenerative diseases, and recent research has demonstrated its potential in alleviating symptoms and extending lifespan in Huntington’s disease models. This breakthrough offers a glimmer of hope for individuals affected by this devastating genetic disorder, potentially revolutionizing treatment approaches beyond traditional symptom management. The implications of these findings extend to understanding the complex role of glial cells in maintaining neuronal health and the possibility of harnessing their regenerative capabilities for a variety of neurological conditions.
Understanding Huntington’s Disease
Huntington’s disease, or HD as it’s often called, is a tough one. It’s a hereditary disorder, meaning it’s passed down through families. It causes nerve cells in the brain to break down over time. Think of it like a slow, relentless erosion. It impacts movement, cognition, and even a person’s emotional state. Not a pretty picture, right?
The Genetic Basis of Huntington’s
So, what’s the culprit? It all boils down to a single gene, the huntingtin gene. Everyone has this gene, but in people with HD, there’s a mutation – an expanded repeat sequence. Imagine a word being repeated over and over, messing up the whole sentence. The more repeats, generally, the earlier the onset of symptoms. It’s a dominant gene, too, meaning if you inherit it from just one parent, you’re likely to develop the disease. Scary stuff.
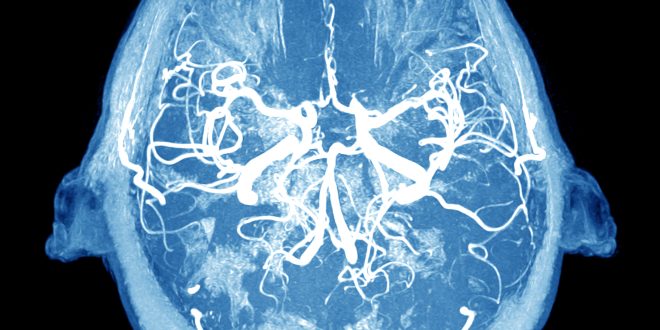
Neurological Impact and Symptoms
The impact on the brain is significant. HD primarily affects the basal ganglia, which controls movement, and the cerebral cortex, responsible for thinking, memory, and perception. As these areas degenerate, you start to see the hallmark symptoms. Uncontrollable movements called chorea are common, along with cognitive decline, depression, and personality changes. It’s a multifaceted disease, attacking from all angles. You know, like some villainous plot from a comic book. Makes you wonder if Dr. Evil was secretly studying neurology, doesn’t it?
Current Treatment Strategies and Limitations
Right now, there’s no cure. Treatments focus on managing symptoms. Medications can help with the chorea and some of the psychiatric issues, but they don’t slow the disease’s progression. Physical therapy, occupational therapy, and speech therapy can provide support and improve quality of life, but again, they’re just band-aids. Honestly, it’s a bit disheartening. It’s like trying to bail water from a sinking ship with a teacup.
The Role of Glial Cells in Huntington’s Disease
Now, let’s talk about the unsung heroes, or rather, the villains in disguise. Glial cells! You probably hear a lot about neurons, the brain’s rockstars, but glial cells? Not so much. But they’re actually super important. They support, protect, and nourish neurons. They’re like the roadies, the security team, and the caterers all rolled into one for the brain’s rockstars. And in Huntington’s, they’re not exactly playing their part well.
Glial Cell Dysfunction in Huntington’s
In HD, glial cells go haywire. They become dysfunctional and can even contribute to neuronal damage. It’s like the roadies deciding to sabotage the band’s equipment. Not helpful! This dysfunction can exacerbate inflammation and impair the brain’s ability to clear out toxic substances. It’s a vicious cycle.
Astrocytes and Huntington’s Pathology
Astrocytes, a type of glial cell, are normally star-shaped (hence the name, “astro”). They’re involved in a whole bunch of important stuff, like regulating the chemical environment around neurons and providing them with nutrients. In HD, astrocytes become reactive and can release inflammatory molecules. They also struggle to perform their usual supportive functions. It’s like they’re so stressed out they forget how to do their jobs. I can relate, honestly.
Microglia and Neuroinflammation
Microglia are the brain’s immune cells. They’re like the cleanup crew, scavenging debris and fighting off infections. But in HD, they can become overactive, leading to chronic neuroinflammation. This inflammation contributes to neuronal damage and disease progression. Think of it as the cleanup crew accidentally setting the building on fire. Overzealous, much?
Glial Cell Transplantation: A Novel Approach
Okay, so here’s where the hope comes in! Glial cell transplantation is a new strategy that aims to replace dysfunctional glial cells with healthy ones. It’s like bringing in a new team of roadies, security, and caterers who actually know what they’re doing. The idea is that these new glial cells can restore balance to the brain and protect neurons from further damage. Sounds promising, right?
The Concept of Glial Cell Replacement
The basic concept is to transplant healthy glial cells into the brain of someone with HD. These cells then integrate into the existing neural circuitry and begin to perform their supportive functions. It’s like giving the brain a fresh start. Could this be the game-changer we’ve been waiting for?
Types of Glial Cells Used in Transplantation
Researchers are exploring different types of glial cells for transplantation, including astrocytes and oligodendrocyte precursor cells (OPCs). OPCs can differentiate into oligodendrocytes, which produce myelin, the insulating sheath around nerve fibers. Replacing damaged oligodendrocytes could improve nerve signal transmission. It’s all about finding the right cells for the job.
Delivery Methods and Engraftment
Getting the glial cells to the right place in the brain is crucial. Delivery methods include direct injection into specific brain regions. Once transplanted, the cells need to engraft, meaning they need to integrate into the surrounding tissue and survive long-term. It’s a bit like planting seeds and hoping they take root. You need the right soil, the right amount of water, and a little bit of luck.
Experimental Evidence: Alleviating Symptoms and Prolonging Life
Now for the exciting part: the evidence! Preclinical studies in animal models of Huntington’s disease have shown that glial cell transplantation can indeed alleviate symptoms and prolong life. This is HUGE. Like finding a winning lottery ticket huge.
Preclinical Studies in Animal Models
Researchers have used mice and other animal models that mimic the symptoms of HD. These studies have shown that glial cell transplantation can improve motor function, reduce neuroinflammation, and slow disease progression. It’s not a cure, but it’s a significant step in the right direction.
Observed Improvements in Motor Function
One of the most striking findings is the improvement in motor function. Animals that received glial cell transplants showed reduced chorea-like movements and improved coordination. It’s like they were given a new lease on life. Seeing is believing, and these studies provide some pretty compelling visuals.
Extended Lifespan in Transplanted Subjects
Perhaps the most significant result is the extended lifespan. Transplanted animals lived significantly longer than control animals. This suggests that glial cell transplantation can not only improve symptoms but also slow the underlying disease process. I mean, who wouldn’t want more time? It’s the one thing we can never get back, right?
Mechanisms of Action: How Glial Transplants Work
So, how does it all work? What’s the magic behind glial cell transplantation? Well, it’s not magic, it’s science! But the exact mechanisms are still being investigated. However, several key factors seem to be at play.
Neurotrophic Support and Neuronal Protection
Transplanted glial cells can provide neurotrophic support, meaning they release factors that promote neuronal survival and growth. They can also protect neurons from toxic substances and oxidative stress. It’s like creating a protective shield around vulnerable neurons.
Modulation of Neuroinflammation
Glial cell transplantation can help to dampen down neuroinflammation. The transplanted cells can release anti-inflammatory molecules and modulate the activity of microglia. This can reduce neuronal damage and promote healing. Basically, the transplanted cells help to calm down the overly aggressive cleanup crew. Good job, team!
Restoration of Synaptic Function
Synapses are the connections between neurons, and they’re essential for communication in the brain. In HD, synaptic function is impaired. Glial cell transplantation can help to restore synaptic function, improving communication between neurons. It’s like fixing a broken telephone line, making sure the message gets through loud and clear.
Challenges and Future Directions
Of course, it’s not all sunshine and rainbows. There are still significant challenges to overcome before glial cell transplantation can become a routine treatment for Huntington’s disease. But hey, nothing worthwhile is ever easy, right?
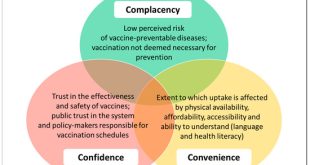
Immunological Considerations and Graft Rejection
One of the biggest challenges is the risk of graft rejection. The recipient’s immune system may see the transplanted cells as foreign and attack them. Immunosuppressant drugs can help to prevent rejection, but these drugs have their own side effects. It’s a balancing act.
Optimizing Cell Source and Delivery
Researchers are working to optimize the source of glial cells for transplantation. Stem cells are a promising source, as they can be differentiated into various types of glial cells. Delivery methods also need to be refined to ensure that the cells reach the right locations in the brain and engraft successfully. It’s all about precision and efficiency.
Translating Preclinical Findings to Clinical Trials
The ultimate goal is to translate the promising preclinical findings into clinical trials in humans. This will require careful planning and rigorous testing to ensure the safety and efficacy of glial cell transplantation. It’s a long road, but the potential payoff is enormous.
Ethical Considerations
With any new therapy, there are ethical considerations to address. Glial cell transplantation is no exception. It’s essential to proceed responsibly and thoughtfully.
Informed Consent and Patient Selection
Patients participating in clinical trials need to be fully informed about the potential risks and benefits of glial cell transplantation. Patient selection criteria need to be carefully defined to ensure that the most appropriate individuals are included in the trials. Transparency is key.
Long-Term Monitoring and Potential Risks
Long-term monitoring is essential to assess the safety and efficacy of glial cell transplantation. Potential risks, such as tumor formation or unexpected side effects, need to be carefully monitored. It’s a marathon, not a sprint.
Accessibility and Equity in Treatment
If glial cell transplantation proves to be an effective treatment for Huntington’s disease, it’s important to ensure that it’s accessible to all patients who could benefit, regardless of their socioeconomic status. Equity in healthcare is a fundamental principle.
Glial cell transplants are showing a lot of promise in the fight against Huntington’s, and it’s cool to see science pushing boundaries. It offers a real chance to improve lives and maybe even find a cure one day. It’s definitely something to keep an eye on and discuss with your doctor if you or someone you know is affected by HD. Who knows? Maybe this is the turning point we’ve all been waiting for!
 Cloudabouts
Cloudabouts